Postpartum hemorrhage
Postpartum hemorrhage is one of the leading causes of maternal death in the state of Santa Catarina, Brazil, and worldwide.Based on the “ASSISTANCE RECOMMENDATIONS FOR THE PREVENTION, DIAGNOSIS, AND TREATMENT OF OBSTETRIC HEMORRHAGE,” we propose simulation for the treatment of this condition.
Target Audience: Medical and nursing students/residents, and healthcare professionals.
Simulation Location: This simulation is planned to take place in the work environment. It is a simulation modality called “in-situ simulation.” It is important to assess problems and difficulties that occur in the real environment.
Objectives: Training for effective management of postpartum hemorrhage.
Required Materials:
- Materials available in the department – preferably two 500ml IV fluids and one 100ml IV fluid with administration sets for use in the simulation.
- Indwelling urinary catheter + drainage bag
- Sheet with “blood” stains – previously painted with red and black fabric paint
- Neoprene uterus or partially deflated beach ball
- Baby doll or simulator
- Posters or papers with Blood Pressure and Pulse measurements.
Preparation: Choosing the appropriate time and place is crucial to avoid interfering with patient care is essential, in an in situ simulation. It is important to coordinate in advance with the healthcare team and supervisors. Coordinate the use of supplies, the location, and the presence of learners. Choose a bed or postpartum room and place the sheet. Invite one of the participants to act as the postpartum woman – explain what will happen.
Briefing: Explain to the participants what will happen, what is expected of them, and how they will be evaluated. Create a protected and respectful environment. Ensure appreciative feedback. If photography is planned, ask for and obtain consent for image use beforehand.
Participant Distribution: Apart from the patient, at least one nurse, one doctor, and one or two additional professionals should be chosen to assist in the next steps. There may be an accompanying person. Other participants are invited to evaluate the simulation using checklists for technical and non-technical skills.
Clinical Scenario: G2P1 woman underwent cesarean section for arrest of descent after two hours of pushing. The baby weighs 4000g. The surgery was uneventful. Two hours post-surgery, she was discharged from recovery and is in the postpartum room. The nurse assesses vital signs. The patient is anxious with mild shortness of breath. Assessing increased vaginal bleeding. (Show vital signs poster) BP=100/60mmHg / HR=110 bpm
Simulation: Allow participants to conduct the simulation – assist only if necessary. Consider timing the request for a specific action (e.g., oxytocin) and its simulated “infusion.” Depending on the simulation, allow vital signs to improve or worsen. Ask non-participants to fill out the checklists.
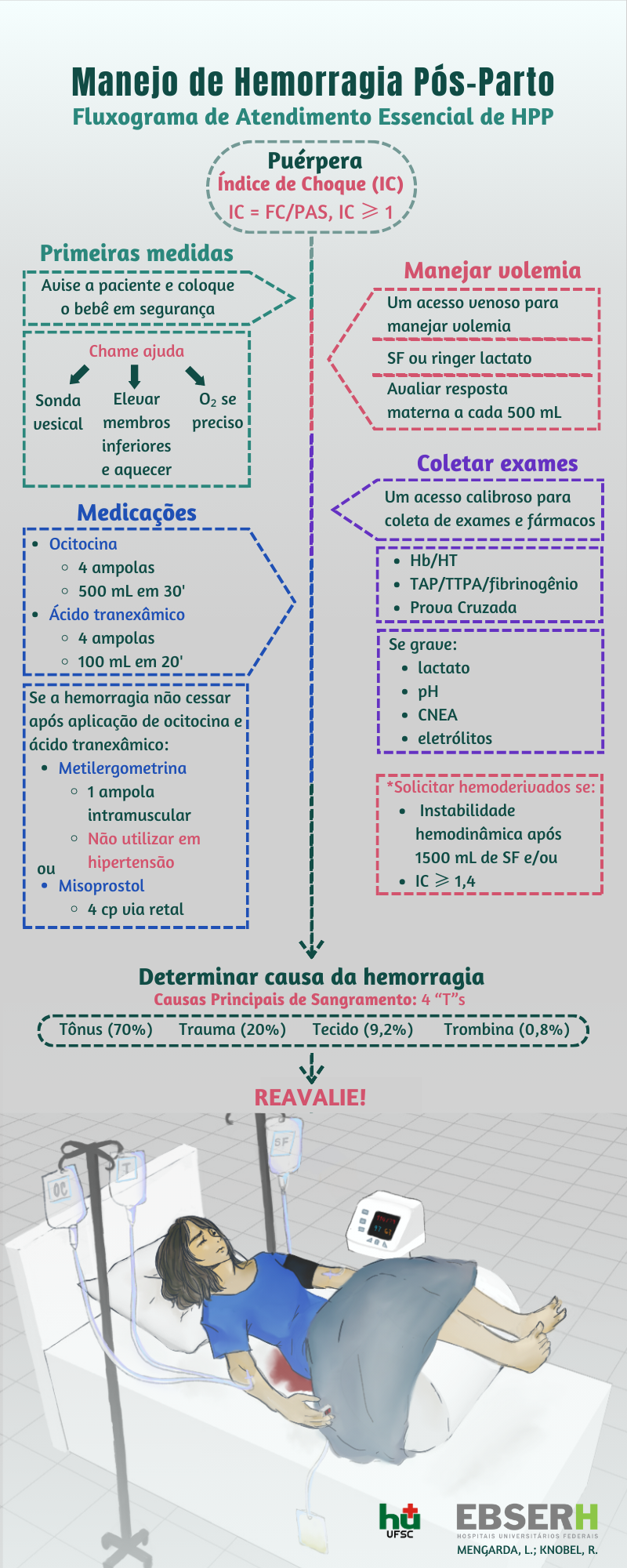
Debriefing: Start debriefing with the patient – how she felt, what was good, and what was not (in that order). If communication occurred, what was communicated, if she felt well cared for. Then move on to the healthcare professionals (starting with what they did well) and finally the audience. Always begin with positives and provide constructive criticism. Encourage everyone to suggest improvements. Based on the simulations, we have created the poster and the folder.
Based on the simulations, we created:
And:








